This study explored the role of psychological safety (PS) on team performance (both perceived and actual performance) in the intensive care unit (ICU).
Daily surveys of healthcare providers in 12 ICUs within an integrated health system over a 2-week period were undertaken. Surveys included PS, leader familiarity, leader inclusiveness, role clarity, job strain, and teamwork.
Providing background:
· ICU interprofessional care teams, comprising physicians, nurses, respiratory therapists, pharmacists and other specialised team members, is associated with lower mortality among patients admitted to the ICU
· Despite the demonstrable value of interprofessional teams, little work has focused on how to improve team performance
· Prior work has focused on ICU culture—defined as shares values and beliefs of the ICU staff—however, “most studies of ICU culture have demonstrated no association between culture and ICU quality (6–9). ICU culture is also a vague concept, without clearly actionable targets for improvement” (p1027)
· PS has also been the focus of attention for team performance. PS can be defined as “the condition by which team members feel safe to take risks, explore new ideas, and challenge the status quo” (p1028)
· PS could “manifest as team members with a low position on the hierarchy challenging treatment plans or speaking up about failures to deliver evidence-based care” (p1028) and in some earlier work, has been associated with greater engagement in quality improvement
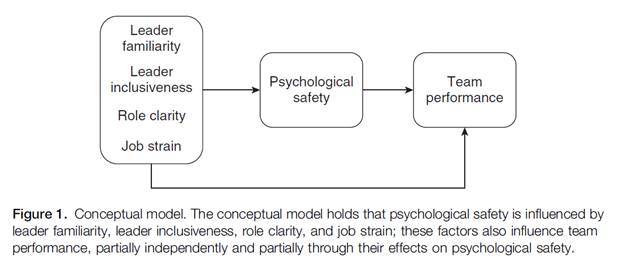
They provide their conceptual model below:
Results
Key findings included:
· At the individual level – high leader inclusiveness and lower job strain were independently associated with greater PS
· Higher PS was independently associated with greater perception of teamwork
· However, there was no association between team PS and actual performance on mechanical ventilation tasks
· They conclude that “Psychological safety is associated with several modifiable factors in the ICU but is not associated with actual use of evidence-based practices”
Expanding on the findings, team members’ beliefs about PS were positively associated with perceived leader inclusiveness and negatively associated with job strain.
Moreover, team members’ beliefs about PS were positively associated with greater perceived teamwork in the ICU, however this did not flow into differences in actual team performance when measured via mechanical ventilation practices.
Role clarity was associated with both PS and teamwork in the unadjusted models, but wasn’t statistically significant when adjusted for the full factors. Leader familiarity wasn’t associated with either PS or teamwork.
They argue that this data identifies a strategy for improving PS and teamwork – via greater use of inclusive behaviours by intensivists on rounds.
Inclusive behaviours “might include pausing during discussions to give space for others’ contributions, actively soliciting input from other team members, explicitly justifying key decisions so team members understand their rationale, and vocally admitting when uncertainty exists to create a safe place for disagreement” (p1032).
This data also expands a little on how job strain may affect care. Time pressure is well known to impact individual decisional capacity interaction and thus, job strain via time pressure and other mechanisms “might negatively impact teamwork both directly (e.g., by reducing time for effective collaboration) and indirectly (e.g., by reducing the time for behaviors that engender psychological safety)” (p1032).
Job strain was independently associated with worsened perceptions of teamwork even when controlling for PS.
Moreover, leader familiarity in the context of the ICU wasn’t necessary for effective teamwork. For ICUs, team composition is not typically planned (but rather ad hoc), and of low temporal stability. [** these findings may not necessarily extend to other contexts outside of ICU and healthcare.]
Finally, while PS was strongly associated with perceived teamwork, they found no evidence that stronger PS influenced actual practices (mechanical ventilation). They provide some explanations why this may be the case:
1) Since PS was already high, perhaps there was insufficient variation to detect an association
2) The two practices chosen may not have been as dependent on team performance as the authors hypothesised
3) Possibly ventilation management is so protocolised that they aren’t that dependent on teamwork
Several limitations were of course present.
Authors: Diabes, M. A., Ervin, J. N., Davis, B. S., Rak, K. J., Cohen, T. R., Weingart, L. R., & Kahn, J. M. (2021). Annals of the American Thoracic Society, 18(6), 1027-1033.
Study link: https://doi.org/10.1513/AnnalsATS.202006-753OC
LinkedIn post: https://www.linkedin.com/pulse/psychological-safety-intensive-care-unit-rounding-teams-hutchinson
2 thoughts on “Psychological Safety in Intensive Care Unit Rounding Teams”