This systematic review evaluated evidence for what support staff want vs what they receive, and whether the support is effective. 99 studies were included.
Some extracts:
· PSI (patient safety incident) lead to emotional shame, guilt, anger, shock, depression, fear, flashbacks, helplessness, fatigue, withdrawal and more
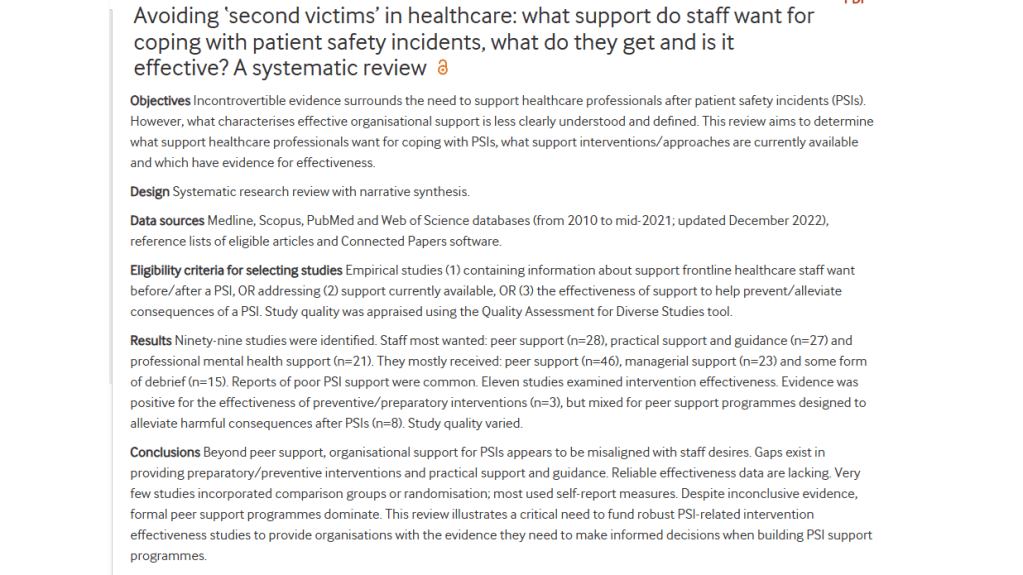
· The three most desired support types staff want before and after a PSI are peer support, practical support and guidance, professional mental health support
· In contrast, the three support types staff receive prior to and following a PSI are peer support, managerial support and post-incident debrief
· “healthcare professionals want organisational support at multiple levels: a supportive and learning oriented culture (primary prevention level support), peer support, practical support and guidance, post-incident debriefing to clarify and process what happened (secondary level support) and access to professional mental health support (tertiary level support)”
· “However, there is limited evidence that organisations are giving staff what they want: overwhelmingly, organisational support for PSIs is perceived as inadequate, non-existent or dependent on one’s organisational status”
· “Where support is provided, secondary-level approaches dominate—largely at a local level from peers and one’s line manager”
· “There is a gap in primary-level (preparatory, proactive, preventive) approaches, which tend to be missing from staff reports”
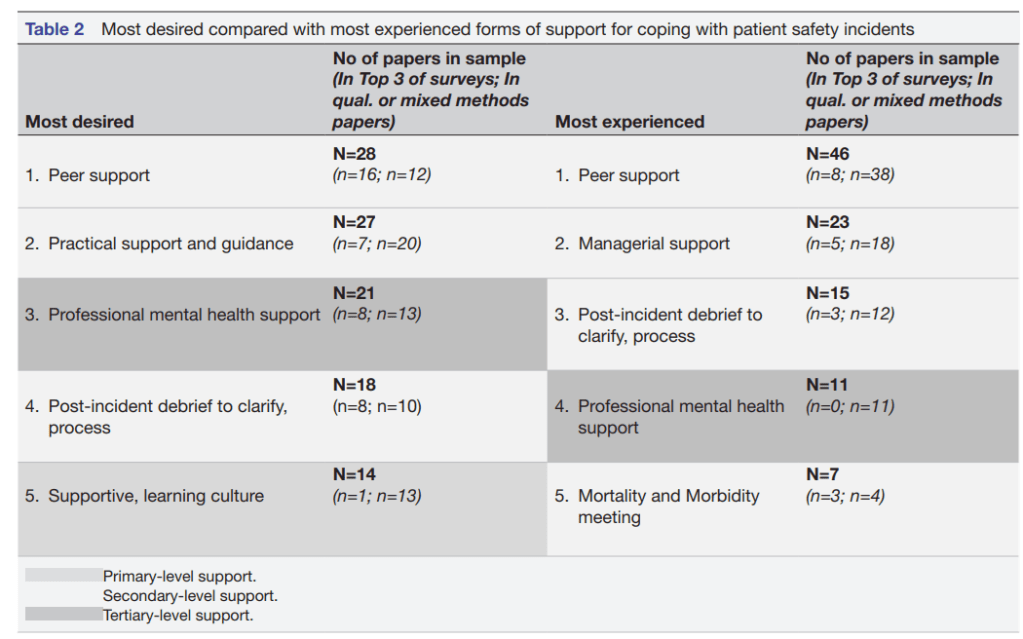
How effective are the support interventions?
· For primary-level/preventative, evidence was “largely positive for the effectiveness of the three primary-level interventions in preparing healthcare staff and trainees for exposure to adverse events”
· “All three studies reported significant improvements in targeted outcomes, particularly in relation to knowledge and awareness of resources in relation to the second victim phenomena online supplemental table”
· Evidence for effectiveness of secondary-level interventions was mixed
· Better evidence is behind primary interventions designed to “equip and prepare staff for involvement in PSIs, than for secondary interventions, which aim to mobilise support and promote staff coping after involvement in a PSI”
· Secondary-level interventions still dominate the literature, e.g. “popular peer support programmes, which have mixed evidence regarding their effectiveness”
· “it is noteworthy that the interventions and approaches within our sample tended to target the individual, rather than focusing on teams (where incidents happen and must be dealt with)”
· And “the emphasis appears to be on reducing distress after a PSI, trying to ‘fix what has gone wrong in the healthcare provider’”
· “primary interventions may be more effective at stress reduction than secondary or tertiary approaches [and] multilevel intervention strategies combining individual-level and organisational-level interventions are more effective than uni-level interventions alone,79 81 82 therefore organisations risk poorer returns on their investment if they fail to adopt a comprehensive approach”
· “Primary-level interventions, particularly those addressing improvements in culture and working practices, appear to be especially important in healthcare settings, because of the significant impact the presiding patient safety culture has on staff’s recovery trajectory after a PSI”
· “Organisations that fail to invest in primary-level support—specifically, implementing a fair and just organisational culture—but provide a formal peer support programme (secondary level) or EAP (tertiary level), risk staff viewing these provisions as ‘tokenistic’, or as signifiers that the organisation has abdicated responsibility for its staff because it is not tackling poor culture which is a major source of distress”
· “when employers ask their staff to identify factors that would have the greatest impact on their well-being at work, they overwhelmingly suggest better communication, staffing and interpersonal connectivity, rather than issues targeted by well-being programmes”
Ref: Simms-Ellis et al. (2025). Avoiding ‘second victims’ in healthcare: what support do staff want for coping with patient safety incidents, what do they get and is it effective? A systematic review. BMJ open, 15(2), e087512.

Study link: https://doi.org/10.1136/bmjopen-2024-087512
