This may interest people – a meta-analysis and systematic review of the effects night shift work has on markers of cardiovascular risk.
Not a summary – you can read the full open access paper.
81 studies met inclusion criteria – 14 cohort and 67 cross-sectional.

Findings:
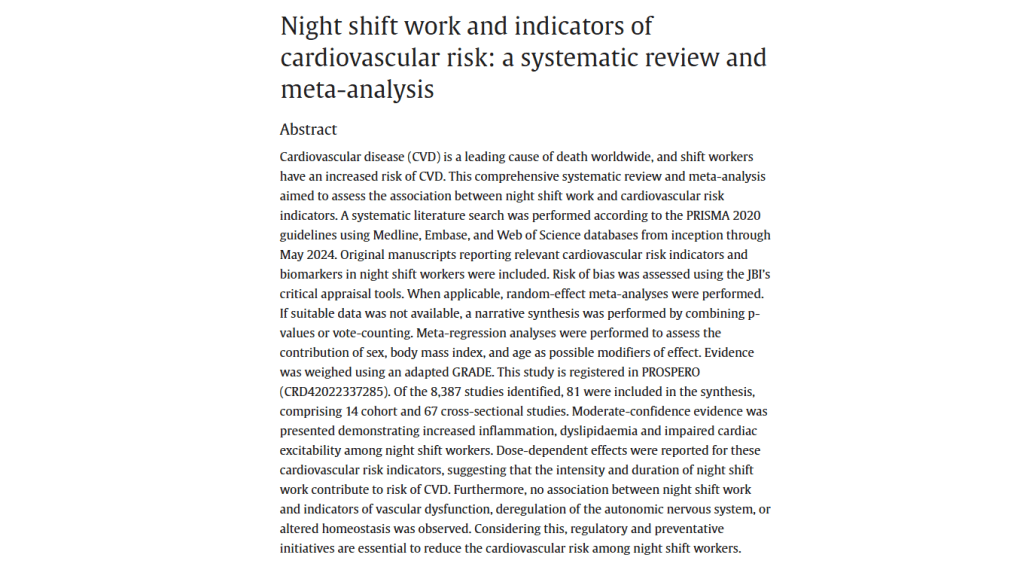
· “Night shift work is associated with increased inflammation
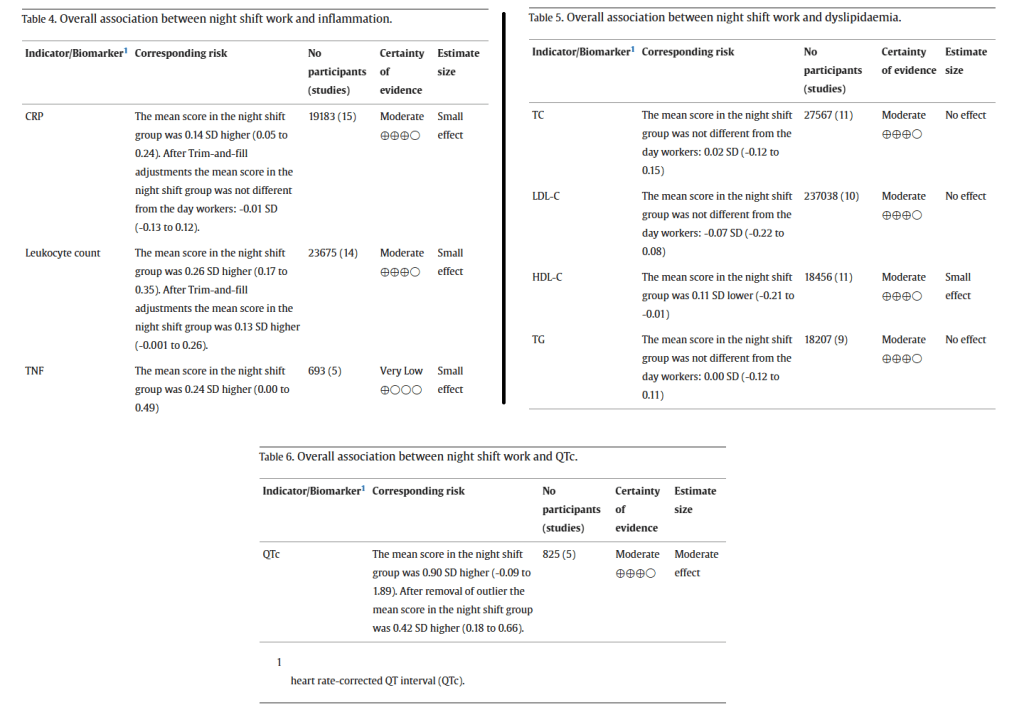
· “HDL-C levels are decreased among night shift workers”
· “Night shift workers have prolonged heart rate-corrected QT intervals (QTc)”
· “HDL-C and QTc are promising indicators of CVD risk among night shift workers”
· “Dose-dependent effects were reported for these cardiovascular risk indicators, suggesting that the intensity and duration of night shift work contribute to risk of CVD”
· “no association between night shift work and indicators of vascular dysfunction, deregulation of the autonomic nervous system, or altered homeostasis was observed”
· “Considering this, regulatory and preventative initiatives are essential to reduce the cardiovascular risk among night shift workers”
· “A positive association was observed across all inflammation biomarkers but especially prominent for leukocyte counts. Furthermore, dose-dependent effects have been reported for CRP and leukocyte counts, with increasing CRP and leukocyte counts according to working duration”
· “the observed heterogeneity for leukocyte counts could not be explained by age, sex or BMI”
· “However, while inflammatory markers are highly affected by different lifestyle factors, the causality of the effect may be indirect due to changes in lifestyle patterns among night shift workers”
· For dyslipidaemia, “In addition to shift schedule and intensity, duration of night shift work affects the HDL-C levels as increasing duration is associated with reduced HDL-C levels”
· “a dose-dependent effect on QTc max values were reported as increased working duration with night shift work was associated with increasingly prolonged QTc values”
· “Prolonged QTc is associated with an increased risk of arrythmias, and this finding supports a higher cardiovascular burden among night shift workers”
· They note that the direction of causality for prolonged QTc is unknown, since lifestyle factors like diet, sleep and stress are also affected by night shift work
· It’s noted that despite ample evidence of hypertension among shift workers, this study didn’t find associations, nor with arterial stiffness
Ref: Erdem, J. S., Das, M. K., De Ryck, E., Skare, Ø., Jenny-Anne, S. L., Bugge, M., … & Zienolddiny-Narui, S. (2025). Night shift work and indicators of cardiovascular risk: a systematic review and meta-analysis. Environmental Research, 121503.

Study link: https://doi.org/10.1016/j.envres.2025.121503
